Your cart is empty
Free shipping on all US orders


Free shipping on all orders

How much do you know about cholesterol? Most people don’t have the whole picture. It’s absolutely necessary for our existence. Yet, as with anything in excess, bad things can come out of it.
It would be remiss to just assume the facts, however. This is why this guide was created. Let’s take a look at cholesterol in more detail.
Cholesterol is a type of lipid that is essential for building cell membranes, producing hormones, and aiding in digestion. There are broadly two (although VLDL cholesterol also exists) main types of cholesterol: low-density lipoprotein (LDL) and high-density lipoprotein (HDL).
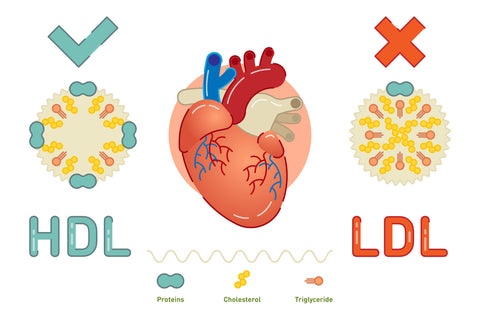
LDL cholesterol is often referred to as "bad" cholesterol because high levels can lead to the buildup of plaque in the arteries, increasing the risk of heart disease and stroke. On the other hand, HDL cholesterol is known as "good" cholesterol as it helps remove LDL cholesterol from the arteries, reducing the risk of heart disease.
Triglycerides are another type of lipid found in the blood. They store excess energy from the diet and are used for energy when needed. High levels of triglycerides can also increase the risk of heart disease.
Remember we mentioned it being essential? Let’s just say that there wouldn't be a you as we know it without cholesterol. Here are some noteworthy roles:
Cholesterol plays a vital role in the formation and maintenance of the structure of cell membranes, which are vital for the functioning of cells in the body.
The structure of cell membranes is a complex and essential aspect of cell biology. Imagine your cell membrane as the gatekeeper of your cells, carefully regulating what goes in and out to maintain a delicate balance necessary for the cell's survival and proper function.
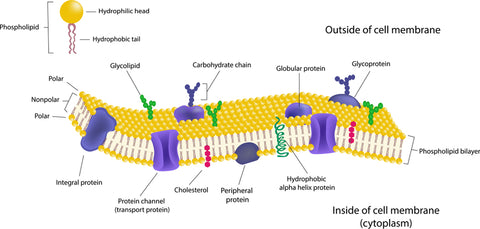
Cholesterol is the architect of the cell membrane, providing structural support and stability. Without cholesterol, the cell membrane would lack the necessary rigidity and flexibility to function effectively. Without cholesterol as the scaffolding, the structure would collapse.
Cholesterol also helps in organizing the various components of the cell membrane. It ensures that different molecules are arranged in the right order, much like organizing books on a shelf for easy access. This organization is vital for the proper functioning of the cell, as it allows for efficient communication between different parts of the cell and with the external environment.
Additionally, cholesterol helps maintain the fluidity of the cell membrane. It acts as a buffer, preventing the membrane from becoming too rigid or too fluid, helping to maintain the consistency. This balance is critical for the cell to respond to its surroundings and carry out essential functions effectively.
Hormone production is another essential process in your body, and cholesterol plays a key role in this mechanism. Cholesterol serves as a building block for the synthesis of important hormones such as estrogen, testosterone, and cortisol. These hormones are vital for maintaining various bodily functions and ensuring overall health and well-being.
Estrogen is a hormone that is primarily associated with female reproductive health. It is responsible for regulating the menstrual cycle, supporting pregnancy, and maintaining bone density. Without sufficient cholesterol levels, your body will struggle to produce an adequate amount of estrogen, potentially leading to hormonal imbalances and related health issues.
Testosterone, on the other hand, is the primary male sex hormone, but it is also present in females in smaller amounts. Testosterone is responsible for regulating libido, muscle mass, bone density, and overall energy levels. Cholesterol acts as a precursor for testosterone production too, highlighting the essential role of cholesterol in maintaining hormonal balance and supporting various physiological functions.
Cortisol is a hormone produced by the adrenal glands in response to stress. It helps regulate metabolism, reduce inflammation, and manage stress levels (under normal circumstances). Cholesterol is necessary for the synthesis of cortisol, emphasizing the interconnected nature of cholesterol and hormone production in your body.
Not surprisingly, inadequate cholesterol intake or synthesis can disrupt the production of these hormones, potentially leading to a range of health issues. Hormonal imbalances can manifest as reproductive disorders, mood swings, fatigue, and metabolic disturbances.
Did you know that Vitamin D is more closely related to a hormone than a true vitamin? As such, it shouldn't come as a surprise that cholesterol plays a crucial role as a precursor for the synthesis of it. When you are exposed to sunlight, particularly UVB rays, a chain of reactions is initiated in your skin. The UVB rays penetrate the skin and interact with a form of cholesterol present in the skin cells. This interaction triggers the conversion of 7-dehydrocholesterol into previtamin D3.
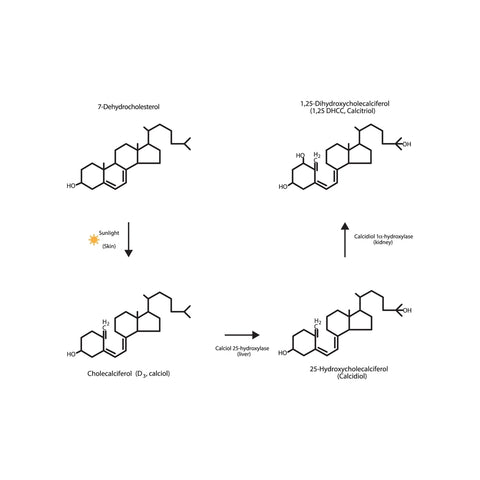
As this previtamin D3 is formed, it undergoes a thermal isomerization process due to body heat, transforming into vitamin D3. This newly synthesized vitamin D3 is then absorbed into the bloodstream, where it travels to the liver for further modification. In the liver, vitamin D3 is hydroxylated to form calcidiol, also known as 25-hydroxyvitamin D.
The journey of vitamin D does not end here. Calcidiol then moves to the kidneys, where it undergoes another hydroxylation process to become calcitriol, the active form of vitamin D. Calcitriol plays a crucial role in regulating calcium and phosphorus levels in your body, which are vital for maintaining strong bones and teeth.
Beyond its role in bone health, vitamin D also plays a significant role in supporting your immune system function. It helps modulate the immune response, enhancing the body's ability to fight infections and diseases. Therefore, ensuring an adequate level of vitamin D through sunlight exposure is crucial for maintaining a robust immune system.
Bile acid synthesis is primarily carried out in the liver, involving the conversion of cholesterol into bile acids, which play a vital role in the digestion and absorption of fats and fat-soluble vitamins in your intestines. The process begins with the uptake of cholesterol from your bloodstream into the liver cells, where it serves as the precursor for bile acid production.
Once inside the liver, cholesterol undergoes a series of complex biochemical reactions to form primary bile acids, such as cholic acid and chenodeoxycholic acid. These primary bile acids are then conjugated with an amino acid, glycine, or taurine to increase their solubility and effectiveness in emulsifying fats. This conjugation process occurs in the liver and is essential for the proper functioning of bile acids in your digestive system.
After conjugation, the bile acids are transported from the liver to the gallbladder for storage. When you consume a meal rich in fats, the gallbladder releases bile into the small intestine to aid in the breakdown and absorption of dietary fats. Bile acids work by emulsifying fats into smaller droplets, increasing the surface area for digestive enzymes to act upon and facilitating the absorption of fatty acids and fat-soluble vitamins like vitamin A, D, E, and K.
In the intestines, the bile acids also form micelles, which are structures that encapsulate lipids and fat-soluble nutrients, allowing them to be transported across the intestinal lining and into your bloodstream. This process is responsible for the efficient absorption of nutrients and plays a crucial role in maintaining overall health.
Your brain is a big blob of fat. Not surprisingly, cholesterol plays a crucial role in brain health. Your brain relies on cholesterol for the formation of synapses, which are essential for communication between neurons and overall brain function. Without cholesterol, the brain would struggle to transmit signals effectively, impacting various aspects of cognitive health.
When you consume foods high in cholesterol, your body transports it through the bloodstream to the brain, where it is utilized in the creation of synapses. These synapses act as bridges between neurons, allowing for the transmission of electrical signals that enable you to think, move, and perform daily tasks.
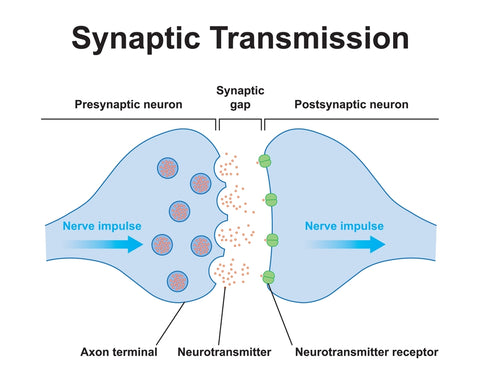
Cholesterol is also involved in the production of myelin, a fatty substance that coats nerve fibers and enhances the speed of signal transmission in the brain. This myelin sheath is needed for efficient neural communication, ensuring that your brain functions optimally.
It is important to note that while cholesterol is necessary for brain health, an imbalance can have negative consequences. High levels of LDL cholesterol can lead to the buildup of plaques in the arteries supplying the brain, restricting blood flow and potentially increasing the risk of cognitive decline.
When a wound occurs, your body initiates a complex process to repair the damaged tissues and restore normal function. Cholesterol is a key component of cell membranes and is essential for their structural integrity. During wound healing, your body requires even more cholesterol to support the growth and division of cells involved in the repair process, as well as to repair the damage to cell membranes.
One of the primary mechanisms behind cholesterol’s action on wound healing is its role in cell signaling. Cholesterol-rich lipid rafts in cell membranes serve as platforms for signaling molecules that regulate various cellular processes, including inflammation, cell migration, and proliferation. These signaling pathways are vital for coordinating the different stages of wound healing, from the initial inflammatory response to the formation of new tissue.
Cholesterol also contributes to the production of important compounds called oxysterols, which help to modulate the inflammatory response and promote tissue regeneration. By influencing the activity of immune cells and growth factors, oxysterols help regulate the balance between inflammation and tissue repair, ensuring that the wound healing process progresses effectively.
Furthermore, as we discussed, cholesterol is a precursor for the synthesis of steroid hormones, such as cortisol and estrogen, which play significant roles in wound healing. These hormones have immunomodulatory effects and can regulate the inflammatory response to prevent excessive tissue damage while promoting the formation of new blood vessels and collagen synthesis.
More than this, it is also involved in the formation of lipid mediators that regulate vascular permeability, platelet function, and immune cell recruitment to the site of injury. These lipid mediators help create a favorable environment for tissue repair by promoting angiogenesis, clot formation, and the removal of debris from the wound site.
Even though it is exceedingly important, there are many instances of high cholesterol contributing to, or causing health issues too. These are the ones to keep an eye out for:
Heart disease is a serious health concern that can be influenced by various factors, with one of the key ones being the levels of LDL cholesterol in your body. When the levels of LDL cholesterol are high, it can contribute to the accumulation of plaque in your arteries.
This buildup of plaque can narrow the arteries, reducing blood flow to the heart and other vital organs. As a result, you may be at a higher risk of developing heart disease and experiencing potentially life-threatening conditions like heart attacks or strokes.

It is essential to understand the impact of LDL cholesterol on your cardiovascular health. High levels of LDL cholesterol can cause inflammation in the arteries, making them less flexible and more prone to damage.
This can further contribute to the formation of blood clots, which can block the flow of blood to your heart or brain, leading to severe complications. The presence of excess LDL cholesterol in your bloodstream can also trigger the accumulation of fatty deposits in the arteries, a process known as atherosclerosis.
Elevated cholesterol levels even play a significant role in the development of hypertension, although the two might not appear to be related in any form. However, hypertension is a critical health concern as it is a major risk factor for various cardiovascular diseases, including, but not limited to heart disease and stroke.
In excess, cholesterol can lead to the formation of plaque on the walls of your arteries. This buildup of plaque can narrow the arteries, causing an increase in blood pressure. The heart then has to work harder to pump blood through the narrowed passageways, resulting in elevated blood pressure levels.
High blood pressure can cause damage to the arteries over time, making them more prone to atherosclerosis, further restricting blood flow. Hypertension can also place additional strain on the heart muscle, leading to conditions like an enlarged heart, or heart failure if it is unable to keep up with the demands placed upon it.
Regular monitoring of blood pressure and cholesterol levels is important for early detection and management of hypertension. High blood pressure might be deadly, but it is also a highly preventable cause of premature death.
While obesity and high cholesterol levels are not inextricably linked, there is a strong correlation as it related to dietary consumption of cholesterol-laden foods and weight gain.
Diets that are rich in their supply of cholesterol usually also share the distinction of being high in saturated fat.
Saturated fats are well-established to have a negative effect on health when consumed in excess. It is important to stress the “in excess” part since we are not trying to peddle a low-fat conspiracy.
These fats are typically found in animal products, but also in some plant-based oils. When you consume high levels of saturated fats, your body may store the excess calories as fat of its own, contributing to weight gain and an increased predisposition to obesity.
Obesity is far more than a cosmetic complaint. It is a complex health issue that can have far-reaching consequences on your well-being. In addition to increasing your risk of heart disease, obesity is also associated with a higher likelihood of developing metabolic conditions such as type 2 diabetes, high blood pressure, and even certain types of cancer.
Lean, our flagship weight loss aide can help you utilize calories faster and reduce the subsequent storage of fat. Combine with exercise and a healthy diet for best results.
Liver issues can arise when high cholesterol levels trigger a condition known as non-alcoholic fatty liver disease (NAFLD). We have covered this topic before at length since it is a prevailing health condition that requires your attention.
However, in a nutshell, this condition occurs when excess fat builds up in the liver, hindering its normal function. The liver, a vital organ in your body, plays a crucial role in processing nutrients, filtering blood, and detoxifying harmful substances. When fat accumulates in the liver cells, it can lead to inflammation, scarring, and ultimately, impair the liver's ability to perform these essential functions.
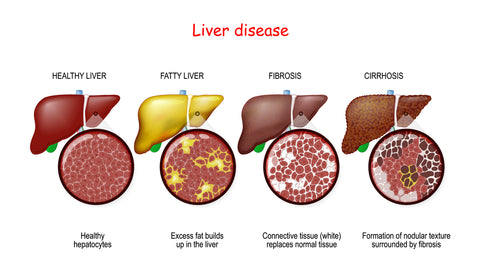
Non-alcoholic fatty liver disease often develops silently, without noticeable symptoms in the early stages. Over time, however, it can progress to more severe conditions such as liver fibrosis and cirrhosis. Fibrosis occurs when the liver tissue becomes scarred, impacting its ability to function properly. Cirrhosis, a more advanced stage, involves extensive scarring that can lead to liver failure and other serious complications that require hospitalization and urgent medical care.
Several factors can contribute to the development of non-alcoholic fatty liver disease, with high cholesterol levels being one of the primary risk factors. Unhealthy dietary habits, a sedentary lifestyle, obesity, insulin resistance, and genetics can also play a role in the onset and progression of this condition.
Managing cholesterol levels through lifestyle modifications, such as adopting a healthy diet and engaging in regular physical activity, is crucial in preventing and managing liver issues associated with high cholesterol.
Most people do not have an understanding of the intricacies of cholesterol levels. While diet plays a role in cholesterol levels, genetics, and other factors also influence your cholesterol profile- sometimes so much that it can override healthy dietary practices.
This is why consideration needs to be given to the family history of the patient, as mere restriction of dietary fat might not be sufficient to curtail hypercholesteremia with a strong familial link.
Understanding your cholesterol levels is the first step in maintaining good heart health. When you get your cholesterol levels checked, you will receive a scorecard that includes several numbers. One of the key numbers to pay attention to is your total cholesterol level, which is the sum of your LDL and HDL cholesterol levels, along with 20% of your triglyceride reading.
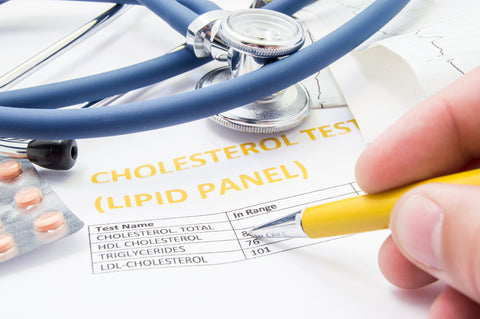
Ideally, your total cholesterol should be below 200 mg/dL. Another important number is your LDL cholesterol level, with levels below 100 mg/dL considered optimal for most people. Conversely, higher levels of LDL cholesterol can increase your risk of heart disease.
Testing for cholesterol is typically recommended for adults starting at age 20. However, if you have risk factors for heart disease such as a family history of high cholesterol or heart attacks, your healthcare provider may recommend earlier and more frequent testing. The test, known as a lipid panel (or lipid profile), requires fasting for 9 to 12 hours before blood is drawn to get accurate results.
Remember, cholesterol levels can fluctuate based on various factors like diet, exercise, and genetics. Maintaining a healthy lifestyle by eating a balanced diet, exercising regularly, and avoiding smoking can help keep your cholesterol levels in check. If your cholesterol levels are outside the optimal range, your healthcare provider may recommend lifestyle changes, medications, or a combination of both to lower your risk of heart disease.
Managing your cholesterol levels is an absolute necessity if you are serious about maintaining good health. Wondering how you can help manage your cholesterol before it goes awry? Let’s check out some of the best strategies.
You didn't think that you were allowed free reign to eat whatever you wanted and have perfect cholesterol, did you? One of the most effective lifestyle changes to manage healthy cholesterol levels is to adopt a diet that is low to moderate in saturated fat, and rich in fiber, whole grains, lean proteins, and healthy fats such as those found in fish, nuts, and certain vegetable oils.
The Mediterranean diet, which emphasizes fruits, vegetables, whole grains, legumes, and olive oil, has been shown to be particularly beneficial in reducing LDL cholesterol and increasing HDL cholesterol. It is an excellent example of what to follow to get control of your values. Limiting the intake of red meat, processed foods, and sugary drinks can also do their part to help maintain healthy cholesterol levels.
Regular physical activity can help offer the double whammy of raising HDL cholesterol levels and reducing LDL cholesterol. Engaging in at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous-intensity exercise per week can significantly improve cholesterol levels. Activities such as brisk walking, swimming, cycling, or dancing can be easily incorporated into daily routines.

Don’t forget to add, resistance training exercises to the mix, since they can help increase muscle mass and boost metabolism, contributing to better cholesterol management.
Even though we said they aren’t mutually exclusive, being overweight or obese can lead to higher levels of LDL cholesterol and lower levels of HDL cholesterol. Losing excess weight through a combination of a balanced diet and regular exercise can help improve cholesterol levels and reduce the risk of heart disease.
Even a modest weight loss of 5-10% of body weight can have significant benefits for cholesterol management. It is important to set realistic weight loss goals and adopt sustainable lifestyle changes to maintain a healthy weight in the long term.
Smoking has a significant impact on lowering HDL cholesterol levels and increasing the risk of heart disease. Quitting smoking can help raise HDL cholesterol and improve overall cardiovascular health. If quitting is difficult, seeking support from healthcare professionals or smoking cessation programs can be beneficial.
Likewise, excessive alcohol consumption can raise triglyceride levels and contribute to unhealthy cholesterol levels. Limiting alcohol intake to a moderate amount (up to one drink per day for women and up to two drinks per day for men) can help maintain healthy cholesterol levels. There is little evidence that shows red wine as being heart-healthy, but the key remains moderation. A bottle of wine a day won’t do any favors for your heart!
It is said that fiber acts as a sponge, reducing LDL cholesterol by binding to it in the digestive tract and promoting its excretion from the body. Good sources of soluble fiber include oats, barley, citrus fruits, apples, beans, lentils, and peas.
Aim to consume at least 5-10 grams of soluble fiber per day to see cholesterol-lowering benefits. Gradually increasing fiber intake and drinking plenty of water is recommended as opposed to going for the max, as it can help prevent digestive discomfort.
Taking Field of Greens as part of your daily morning ritual is an easy way to get some more dietary fiber to assist with cholesterol management and bowel regularity.
Plant sterols and stanols are natural compounds found in small amounts in fruits, vegetables, nuts, and seeds. They have a structure similar to cholesterol and can help block its absorption in the intestines.
Many food products, such as margarine, yogurts, and orange juice, are now fortified with plant sterols and stanols. Consuming 2-3 grams of these compounds per day can help lower LDL cholesterol levels.
Replacing some animal proteins with plant-based proteins can help lower LDL cholesterol as well. Good options include legumes, nuts, seeds, and soy products like tofu and tempeh (when applicable).
Fatty fish, such as salmon, mackerel, and sardines, are also excellent choices as they provide omega-3 fatty acids that can help raise HDL cholesterol and reduce inflammation. When consuming animal proteins, opt for lean cuts of meat and remove visible fat and skin from poultry.
Smart supplementation, such as adding whey or collagen protein can also help support your metabolic rate and lean mass gain.
Diets high in added sugars and refined carbohydrates can contribute to elevated triglyceride levels and lower HDL cholesterol. Foods such as sugary drinks, candy, baked goods, and white bread should be limited.
Instead, choose complex carbohydrates like whole grains, fruits, and vegetables, which provide fiber, nutrients, and slower-releasing energy. When reading food labels, be mindful of added sugars, which can have many different names, such as high-fructose corn syrup, sucrose, and dextrose to name a few.
Familial or genetic factors play a significant role in the development of high cholesterol levels, unbeknownst to many people. Certain genetic variations can affect the body's ability to metabolize and regulate cholesterol, leading to elevated levels in the bloodstream.
One of the most well-known genetic conditions is familial hypercholesterolemia (FH), an inherited disorder characterized by extremely high levels of low-density lipoprotein (LDL) cholesterol from birth. Individuals with FH have a defect in the LDL receptor gene, which impairs the body's ability to remove LDL from the blood, resulting in a buildup of cholesterol.
Other genetic polymorphisms in various genes involved in cholesterol metabolism, such as APOB, PCSK9, and LDLR, have also been implicated in an increased risk of high cholesterol. These genetic variations can lead to reduced clearance of LDL cholesterol or increased production of cholesterol in the body. Individuals with a family history of high cholesterol or premature heart disease are more likely to have a genetic predisposition to developing high cholesterol themselves.
It is important to note that while genetic factors contribute to high cholesterol, lifestyle factors such as diet and physical activity also play a crucial role in managing cholesterol levels. Individuals with a genetic predisposition to high cholesterol may need to be more vigilant in adopting healthy lifestyle habits and may require medication to control their cholesterol levels effectively.
Genetic testing can help identify individuals at high risk for developing high cholesterol, allowing for early intervention and management to reduce the risk of cardiovascular disease.
Cholesterol can be considered a double-edged sword, of sorts. It is an extremely necessary weapon for the health and normal functioning of our body, yet, it can turn around and contribute to significant damage if not kept in check.
The good news is that you can turn things around if they aren’t looking good. The important thing is that you are able to see when something is going wrong early on. FH might be a challenge, but with medical care and diligent following of treatment protocols, you can keep your values in a normal range.